Over the last few years, our blogs have consistently noted the problematic issues faced in the U.S. healthcare industry. Simultaneously, we have also discussed the opportunities to make substantive changes that would not only improve the quality of care, but also reduce cost. After studying over 30+ years encompassing all aspects of healthcare, we have never been more convinced that if we cannot achieve both, then we cannot achieve this goal all together.
In this series of blogs, we have chosen to explore the continuing opportunity to improve the quality of care for Medicare patients (those over the age of 65). Due to the growing numbers in the system, if we cannot reduce cost in healthcare, we need to strive for some cost containment and control. As we have discussed many times in our previous blogs, to improve both the quality of care and reduce cost collectively, we must make material investments in technology and multiply the consumers’ engagement in managing their own health.
The current Medicare Advantage program in the United States should be celebrated, expanded, and heralded as a great success! Under Medicare Advantage, seniors can join a healthcare company-sponsored program, that in ALL cases provides more benefits either at the same cost as Medicare, or in many cases, at a much lower cost. In some cases, as well as communities, Medicare beneficiaries receive a reimbursement of the monthly Medicare Part D cost as part of joining these Medicare Advantage programs. It is a program that we have felt so strongly about that we have recommended it to our own family members over the last two decades.
First, a little history…Medicare Advantage was first a pilot program in South Florida and eventually evolved into Medicare Part C. In the federal program, paid through Medicare, insurance companies received a capitation, or flat rate per patient based on a complicated matrix of patient demographics and health conditions, and insurance companies are then responsible for effectively all the care and all the medical cost of the beneficiary.
The following chart is obvious in showing the growth of Medicare Advantage since 2005 from a baseline of approximately 5 million beneficiaries to over 26 million in 2021.
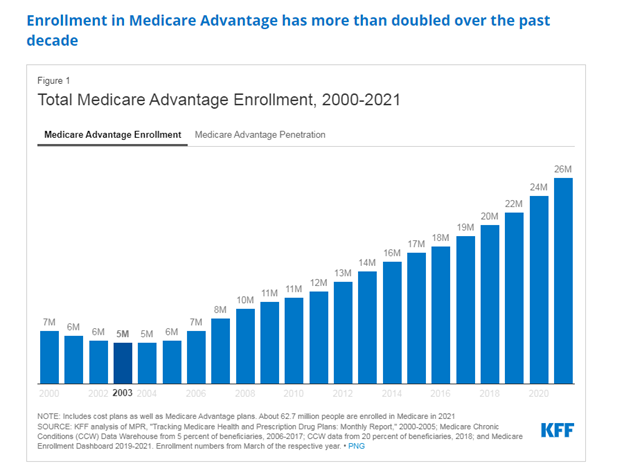
The future is extraordinarily bright for this program and companies have been entering, expanding, or pivoting into this space over the last few years. This pace has accelerated during COVID-19 pandemic and reached new records by the spring of 2021. That trend is not a fad, but the acceleration of the novel product that has reached enough size to virtually guarantee that 50% of all Medicare beneficiaries will be part of the Medicare Advantage program by end of the decade, or in our opinion, sooner than that. The size and scope is incredibly difficult to grasp (more to come in Part 2). Today, Baby Boomers are entering Medicare Advantage at a rate of 50% (of those new enrollees in Medicare) noting the opportunity and value that it provides. It is also much better for planning expenses versus the limitations and 20% co-payment for most of Medicare. We expect that Medicare Advantage will reach 80% of all Medicare beneficiaries by 2035 based on that trend continuing.
As we’ve noted before, this is the only bright spot that we see for providers who have been facing net (inflation adjusted) reductions in Medicare reimbursements for two decades. The transitioning of Medicare beneficiaries to Medicare Advantage requires a change of how the practice is run, such as an increased material investment in people, coupled with a dramatic expansion in the use of technology. Whether the payment model is Medicare Advantage or value-based care, physicians that continue to depend primarily on fee-for-service reimbursements for their survival will be extinct, if not a rare species, during the next 15 years.
More on this topic to come in Part 2.
-Noel J. Guillama, Chairman

